Before considering obesity surgery, one of the first topics your surgeon will discuss is your BMI. This is your Body Mass Index. This simple measurement offers key insights into your overall health. It helps determine if you are a suitable candidate for surgery. In this article, we will explore what BMI is. Discover why it matters, and how it affects your surgical options.
What Is BMI (Body Mass Index)?
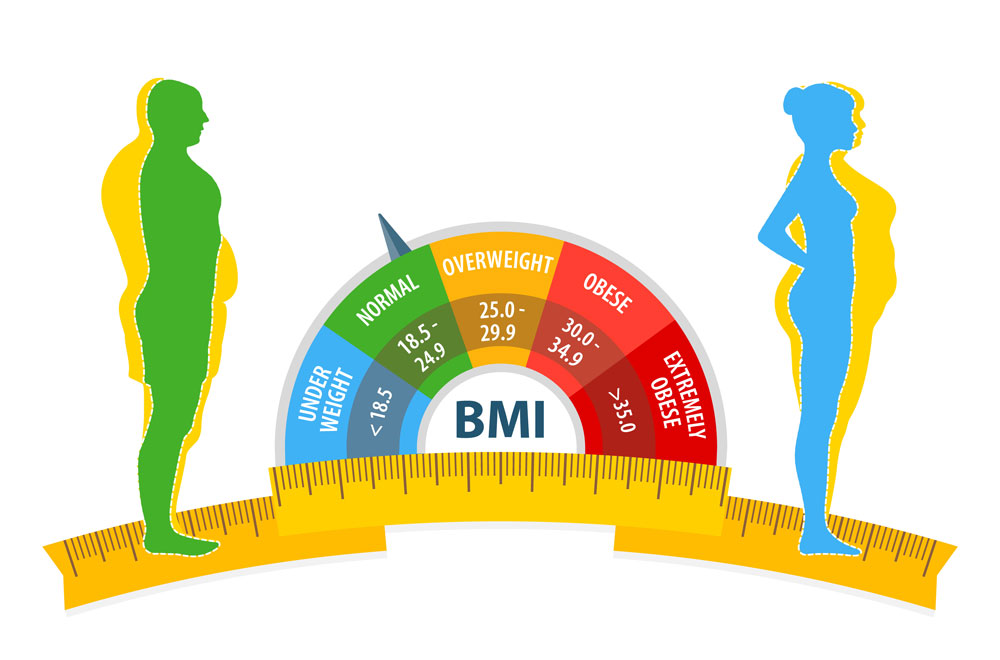
BMI (Body Mass Index) is a tool used to estimate body fat based on height and weight. The formula is simple: your weight in kilograms divided by the square of your height in metres. Although it doesn't measure body fat directly. It offers a quick way to categorise whether you are underweight, normal weight, overweight or obese. This helps doctors assess health risks related to weight.
BMI Categories Explained
The World Health Organisation divides BMI into several categories. A BMI under 18.5 is considered underweight. Between 18.5 and 24.9 is normal weight. From 25 to 29.9 is overweight, while 30 and above is classified as obese. Additionally, obesity is further split into three classes. Class 1 (30-34.9), class 2 (35-39.9), and class 3 (40 and above), often called severe or morbid obesity.
Why Is BMI Important Before Obesity Surgery?
BMI is a key factor in determining eligibility for obesity surgery. Most surgeons recommend surgery for patients with a BMI of 40 or higher. Or 35 and above with obesity-related health issues. A high BMI indicates higher health risks. including diabetes, heart disease and sleep apnoea. Therefore, knowing your BMI helps the medical team tailor the treatment and set realistic goals.
How BMI Influences Surgery Options
Your BMI can affect which surgical procedures are suitable for you. For example, patients with a very high BMI might be better suited for gastric bypass or sleeve gastrectomy rather than adjustable gastric banding. These procedures are more effective for significant weight loss and improving obesity-related conditions. Your surgeon will guide you based on your BMI, lifestyle and health history.
Preparing for Surgery: Beyond BMI
While BMI is important, it is not the only factor surgeons consider. They also assess your overall health, eating habits, psychological readiness and commitment to lifestyle changes. Moreover, you may need to lose some weight before surgery to reduce surgical risks. A dietitian or nutritionist can help create a plan to prepare your body for the procedure.
Can BMI Change Before Surgery?
Yes, many patients are asked to lose some weight before surgery to lower their BMI. Even a modest weight loss can reduce the risk of complications and improve recovery. Additionally, pre-surgery weight loss can show your commitment to making long-term changes. Doctors often provide a specific target weight to achieve before booking the surgery date.
Post-Surgery Weight Loss Expectations
After obesity surgery, your BMI will gradually decrease as you lose weight. The speed and amount of weight loss vary depending on the procedure. It also depends on adherence to dietary guidelines and activity level. Generally, patients can expect to lose 50-70% of excess weight within the first 12 to 18 months. Maintaining these results requires consistent effort, including healthy eating and regular exercise.
Risks of a High BMI During Surgery
A higher BMI can increase surgical risks such as infections, blood clots and delayed healing. Additionally, anaesthesia can be more challenging in patients with higher BMI levels. Because of this, thorough pre-operative assessments and careful monitoring during recovery are essential. Discussing these risks with your surgeon helps you make an informed decision and prepare properly.
Long-Term Benefits of Reaching a Healthier BMI
Achieving a healthier BMI after surgery brings numerous health benefits. It can reduce or resolve type 2 diabetes and lower blood pressure It can also improve heart health and enhance mobility. Furthermore, many patients experience increased energy levels and improved self-esteem. These benefits highlight the importance of maintaining long-term lifestyle changes after surgery.
BMI and Mental Health Considerations
Beyond physical health, BMI is linked to mental health. Obesity can contribute to depression, anxiety and lower self-esteem. Addressing these issues before and after surgery is crucial for overall success. Many clinics offer counselling services to support emotional well-being. Understanding the mental aspects of weight loss helps patients stay motivated and adjust better to their new lifestyle.
Lifestyle Changes After Surgery
After your obesity surgery, maintaining a healthy BMI (Body Mass Index) involves major lifestyle changes. Firstly, following a strict post-surgery diet plan is vital. Gradually, you will transition from liquid to soft foods before returning to regular meals. Portion control becomes a key focus, as your stomach can hold less food. Secondly, regular exercise supports long-term weight maintenance and overall health. Even simple activities like walking or light resistance training can make a big difference. Lastly, attending support groups or therapy sessions can help you stay motivated and address emotional challenges. Adopting these habits ensures the success of your surgery. It will protect your health for years to come.
Conclusion
BMI (Body Mass Index) plays a crucial role in evaluating and preparing for obesity surgery. It helps assess eligibility, select the best surgical approach and plan for recovery. While important, it is just one part of a comprehensive health assessment. Commitment to lifestyle changes, mental readiness and support systems are equally vital. By understanding and managing your BMI, you set the foundation for a healthier future.
For more information on obesity surgery and to book a consultation visit the ACIBADEM Beauty Center Obesity Surgery webpage.
Frequently Asked Questions
No, other factors include overall health, eating habits and psychological readiness.
Sometimes, if you have serious obesity-related conditions. Your surgeon will decide case by case.
Yes, many patients are asked to lose some weight to reduce surgical risks.
Yes, a lower BMI can make recovery smoother and reduce the chance of complications.
Follow a balanced diet, exercise regularly and attend follow-up appointments to stay on track.














